In this detailed exposition, I, Dr. S. Nagendra Boopathy, aim to shed light on calcified coronary artery disease—a condition that poses significant risks to heart health. We will delve into its causes, symptoms, diagnostic methods, and cutting-edge treatment options available today.
Introduction to Calcified Coronary Artery Disease
Calcified coronary artery disease (CCAD) is a significant cardiovascular condition characterized by the accumulation of calcium deposits in the coronary arteries. These deposits lead to the hardening and narrowing of the arteries, restricting blood flow to the heart. Understanding CCAD is crucial for prevention and management, particularly as it can lead to severe complications, including heart attacks.
Understanding Calcium Deposits in Arteries
Calcium deposits in the arteries primarily arise from the body’s natural response to injury. When arteries are damaged due to factors like high cholesterol or inflammation, calcium accumulates as part of the healing process. This buildup can progressively obstruct blood flow and lead to coronary artery disease.
- Formation of Plaque: Cholesterol and other substances combine with calcium to form plaques.
- Calcification Process: Over time, these plaques harden, leading to calcification.
- Impact on Blood Flow: The narrowing of arteries can significantly reduce blood flow to the heart muscle.
The Development of Calcification
The process of calcification in coronary arteries is gradual and can span several years. Initially, smooth muscle cells and macrophages infiltrate the arterial wall, where they eventually undergo apoptosis, or programmed cell death. This cellular death is not random; it is often accompanied by a transformation into calcified structures.
As calcium deposits increase, they can create a rigid environment within the arteries, which complicates the normal function of blood vessels. This rigidity is detrimental, as it leads to increased blood pressure and reduced elasticity of the arteries.
Symptoms of Calcified Coronary Artery Disease
Many individuals with calcified coronary artery disease may not exhibit symptoms until the condition has progressed significantly. Common symptoms include:
- Chest pain or discomfort (angina)
- Shortness of breath during physical activity
- Fatigue
- Heart palpitations
In some cases, symptoms may manifest only during stress or exertion, making it crucial to monitor cardiovascular health regularly.
Diagnosis and Monitoring Techniques
Diagnosing calcified coronary artery disease involves a combination of medical history, physical examination, and advanced imaging techniques. Key methods include:
- Coronary Angiography: This procedure allows visualization of the coronary arteries and the extent of calcification.
- CT Scans: Computed tomography can detect calcium scores, indicating the extent of coronary artery disease.
- Stress Testing: Evaluating heart function under stress can help identify significant blockages.
Regular monitoring is essential for managing and mitigating the risks associated with CCAD.
Traditional Treatment Methods: Bypass Surgery
In cases where calcified coronary artery disease leads to severe blockages, traditional treatment often involves bypass surgery. This surgical intervention aims to create a new pathway for blood flow, bypassing the blocked arteries.
Bypass surgery is typically recommended when:
- The coronary arteries are severely narrowed or blocked.
- Symptoms are persistent and debilitating.
- Other treatment options, such as medication or angioplasty, are not viable.
While bypass surgery can be life-saving, it is essential to consider the risks and benefits carefully. Post-surgery, patients need to commit to lifestyle changes and ongoing medical therapy to manage their heart health effectively.
Advancements in Cardiac Technology
The field of cardiology has seen remarkable advancements in recent years, particularly in the treatment of calcified coronary artery disease (CCAD). These innovations aim to improve patient outcomes and reduce the risks associated with traditional procedures. With the integration of new technologies, cardiologists can now provide more effective and less invasive treatment options.
One of the most significant advancements is the development of specialized devices that facilitate the removal of calcium deposits from the coronary arteries. These devices not only enhance the ability to treat complex cases but also minimize the need for more invasive surgical interventions.
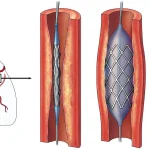
Rotational Atherectomy: A New Approach
Rotational atherectomy is a groundbreaking technique that has transformed the way we approach CCAD. This method employs a diamond-coated burr to effectively remove calcified plaque from narrowed arteries. By rotating at high speeds, the diamond particles can safely grind away calcium, restoring blood flow.
Here’s how it works:
- Preparation: The procedure begins with the insertion of a catheter into the affected artery.
- Rotational Action: The diamond burr rotates at speeds of up to 160,000 RPM, effectively cutting through the calcified deposits.
- Restoration: Once the calcium is removed, the artery is dilated using a balloon catheter, allowing for the placement of a stent if necessary.
This innovative approach is particularly beneficial for patients with heavily calcified arteries where traditional methods may fall short. It offers a viable alternative to bypass surgery, significantly reducing recovery time and improving overall outcomes.
Intra-Vascular Lithotripsy Explained
Intra-vascular lithotripsy is another revolutionary technique that utilizes sonic waves to break down calcified plaques. This method is akin to using shock waves to shatter stones in the kidney, but it is specifically designed for use in the vascular system.
The process involves:
- Balloon Catheter Insertion: A specialized balloon catheter is inserted into the artery.
- Energy Delivery: Once in place, ultrasonic energy is applied, creating microbubbles that collapse and emit shock waves.
- Calcium Fragmentation: These shock waves effectively fracture the calcified deposits, making them easier to treat with conventional angioplasty and stenting.
This technique is particularly advantageous for patients who may not be candidates for traditional procedures due to extensive calcification. It opens new avenues for treatment and enhances the likelihood of successful outcomes.
Patient-Centric Care and Treatment Options
In the evolving landscape of cardiac care, a patient-centric approach is paramount. Each patient’s unique circumstances and preferences must guide treatment decisions. This philosophy ensures that patients are actively involved in their care, leading to better adherence and outcomes.
Options for treatment can vary significantly based on factors such as the severity of calcification, overall health, and patient preferences. Here are some considerations:
- Non-Invasive Options: For patients with mild calcification, lifestyle modifications and medication may be sufficient.
- Minimally Invasive Procedures: Techniques like rotational atherectomy and intra-vascular lithotripsy can be employed for moderate to severe cases.
- Surgical Interventions: In instances where non-invasive methods are not viable, bypass surgery may still be necessary.
Ultimately, the goal is to provide tailored treatment options that align with the patient’s needs and preferences, ensuring the best possible care.
Conclusion and Final Thoughts
Calcified coronary artery disease presents significant challenges, but advancements in cardiac technology have ushered in a new era of treatment possibilities. Techniques such as rotational atherectomy and intra-vascular lithotripsy provide effective alternatives to traditional surgery, improving patient outcomes and reducing risks.
As we continue to refine these methods and explore new technologies, the focus remains on delivering patient-centered care. By prioritizing individual needs and preferences, we can navigate the complexities of CCAD more effectively and enhance the quality of life for our patients.
FAQs about Calcified Coronary Artery Disease
What are the primary causes of calcified coronary artery disease?
Calcified coronary artery disease primarily results from the accumulation of calcium in the arteries, often due to factors such as high cholesterol, inflammation, and arterial damage.
How is calcified coronary artery disease diagnosed?
Diagnosis typically involves a combination of medical history, physical examination, and imaging techniques such as coronary angiography and CT scans to assess calcium buildup.
What are the treatment options for calcified coronary artery disease?
Treatment options vary from lifestyle changes and medication to minimally invasive procedures like rotational atherectomy and intra-vascular lithotripsy, and in some cases, traditional bypass surgery.
Are there risks associated with the new treatment technologies?
As with any medical procedure, there are risks. However, advancements in technology aim to minimize these risks while maximizing effectiveness and patient safety.
How can I prevent calcified coronary artery disease?
Preventive measures include maintaining a healthy diet, exercising regularly, managing stress, and monitoring cholesterol levels to reduce the risk of arterial calcification.