Coronary Artery Bypass Grafting (CABG), commonly known as bypass surgery, is one of the most significant and life-saving procedures in cardiac care. Since its inception in the 1960s, it has revolutionized the treatment of coronary artery disease (CAD), offering hope and improved quality of life to millions worldwide. In this article, we will delve deep into what bypass surgery entails, its history, how it works, who needs it, and the advancements that have made it safer and more effective over the years.
Table of Contents
- Understanding Bypass Surgery: What Exactly Is CABG?
- How Does Bypass Surgery Work?
- Who Needs Bypass Surgery?
- The Impact and Benefits of Bypass Surgery
- Bypass Surgery vs. Stenting: When to Choose What?
- Conclusion: The Legacy of Bypass Surgery
- Frequently Asked Questions (FAQs)
- Final Thoughts
Understanding Bypass Surgery: What Exactly Is CABG?
Bypass surgery is a procedure designed to restore adequate blood flow to the heart muscle by circumventing blocked or narrowed coronary arteries. The heart receives oxygen-rich blood through these arteries, and when they become clogged due to atherosclerosis or other conditions, the heart muscle suffers from reduced blood supply, leading to chest pain (angina), shortness of breath, or even heart attacks.
In simple terms, bypass surgery involves taking a healthy blood vessel from another part of the body and attaching it to the coronary artery beyond the blockage. This creates a new “bypass” route for blood to flow, effectively circumventing the obstructed segment.
The Origin and Evolution of Bypass Surgery
The journey of bypass surgery began in the late 1960s. The pioneering work of surgeons like Dr. René Favaloro introduced the concept of using the left internal mammary artery (LIMA) — a blood vessel that runs along the chest wall — to bypass blockages in the left anterior descending artery (LAD), which supplies a large portion of the heart muscle.
This technique, known as LIMA to LAD anastomosis, is considered the gold standard for coronary revascularization because it has demonstrated long-term durability and excellent patient outcomes. It is often referred to as the “mother of all revascularization” procedures.
Since then, bypass surgery has evolved tremendously with advances in surgical techniques, anesthesia, and postoperative care, making it safer and more accessible to a wider range of patients.
How Does Bypass Surgery Work?
To visualize the concept, imagine a traffic jam on a busy road leading to your destination. To avoid the congestion, an alternate route or bypass is created that allows vehicles to reach the destination without delay. Similarly, in bypass surgery, a new blood vessel is grafted to reroute blood flow around the blocked artery segment.
Surgeons typically use one or more of the following grafts:
- Left Internal Mammary Artery (LIMA): Preferred for bypassing the LAD artery due to superior long-term patency.
- Vein Grafts: Usually the saphenous vein from the leg, used to bypass other blocked arteries.
- Radial Artery: Taken from the arm, this arterial graft can also be used for bypassing coronary arteries.
The grafts are carefully attached to the coronary arteries beyond the blockage, allowing blood to flow freely through the new route. This restores oxygen supply to the heart muscle, alleviating symptoms and reducing the risk of heart attacks.
Types of Bypass Surgery Techniques
Bypass surgery can be performed using different surgical approaches depending on the patient’s condition, surgeon expertise, and available technology:
- Conventional Open-Heart Bypass Surgery: The most common method where the chest is opened through a sternotomy (cutting through the breastbone) to access the heart. The heart may be stopped temporarily, and a heart-lung machine takes over circulation (on-pump surgery).
- Off-Pump Bypass Surgery: Also called beating-heart surgery, this method avoids stopping the heart and using the heart-lung machine, potentially reducing complications.
- Mini-Sternotomy or Minimally Invasive Cardiac Surgery (MICS): Smaller incisions are used, resulting in less trauma and faster recovery.
- Robotic-Assisted Bypass Surgery: Advanced robotic systems allow precise surgery with minimal invasiveness, though this is available only in specialized centers.
Who Needs Bypass Surgery?
Not every patient with coronary artery disease requires bypass surgery. The decision depends on multiple factors evaluated by cardiologists and cardiac surgeons. Key considerations include:
- Extent and Location of Blockages: Patients with multiple blocked arteries, especially involving the left main coronary artery or complex lesions, often benefit more from bypass surgery than from angioplasty or stenting.
- Heart Function: The pumping ability of the heart, measured as ejection fraction, influences treatment choice. Patients with reduced heart function may be better candidates for bypass.
- Presence of Diabetes: Diabetic patients often have diffuse coronary disease and benefit significantly from LIMA to LAD grafting, which offers better long-term outcomes compared to stenting.
- Patient’s Overall Health and Preferences: Age, other medical conditions, and personal choices are vital in planning treatment.
These factors are combined into a comprehensive assessment involving clinical evaluation, imaging studies, and scoring systems like the SYNTAX score, which quantifies the complexity of coronary artery disease. This helps doctors recommend the best treatment—whether bypass surgery, angioplasty, or medical management.
Shared Decision-Making: A Collaborative Approach
Modern cardiac care emphasizes shared decision-making, where physicians provide transparent, scientific information about the benefits and risks of different treatment options. Patients and their families are encouraged to participate actively in choosing the approach that aligns with their values and lifestyle.
This collaborative process ensures that the patient’s preferences and expectations are respected while delivering evidence-based care.
The Impact and Benefits of Bypass Surgery
Bypass surgery has saved countless lives since its introduction. It is especially effective in:
- Relieving angina and improving quality of life.
- Reducing the risk of future heart attacks.
- Enhancing survival rates, particularly in complex coronary artery disease.
The durability of arterial grafts like LIMA to LAD means that many patients enjoy symptom relief and heart function improvement for decades after surgery.
Recovery and Long-Term Outlook
Recovery from bypass surgery varies depending on the surgical technique and patient health. Conventional open-heart surgery typically requires a hospital stay of about a week, followed by cardiac rehabilitation and gradual return to normal activities over several weeks.
Minimally invasive and off-pump surgeries often allow quicker recovery times. Long-term success depends on lifestyle changes, medication adherence, and regular follow-up.
Bypass Surgery vs. Stenting: When to Choose What?
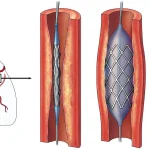
In some cases, less invasive procedures like angioplasty and stenting can open blocked arteries without surgery. However, bypass surgery remains the preferred option when:
- There are multiple blockages or complex lesions.
- Left main coronary artery or proximal LAD artery is involved.
- Patients have diabetes or reduced heart function.
Stenting might be recommended for simpler, single-vessel disease or when surgery poses high risk. The decision is always personalized, based on clinical assessment and patient preference.
Conclusion: The Legacy of Bypass Surgery
Since its inception in the 1960s, CABG or bypass surgery has been a cornerstone of cardiac treatment. The pioneering use of the left internal mammary artery to the left anterior descending artery graft remains one of the most effective procedures in cardiovascular medicine.
Advances in surgical techniques, patient care, and shared decision-making continue to improve outcomes and quality of life for patients with coronary artery disease. Whether through conventional open-heart surgery or minimally invasive methods, bypass surgery offers a life-saving solution that stands the test of time.
For patients and families navigating the complexities of heart disease treatment, understanding the role and benefits of bypass surgery is crucial. It empowers informed choices and fosters hope for a healthier, longer life.
Frequently Asked Questions (FAQs)
What is the difference between bypass surgery and angioplasty?
Bypass surgery involves creating a new route for blood flow around blocked arteries using grafts, while angioplasty opens the blocked artery using a balloon and often places a stent to keep it open. Bypass is more invasive but better suited for complex or multiple blockages.
How long does a bypass surgery last?
The surgery itself usually takes 3 to 6 hours, depending on the number of arteries bypassed and the technique used.
What is the recovery time after bypass surgery?
Recovery can take 6 to 12 weeks after conventional open-heart surgery. Minimally invasive techniques may shorten this period.
Who is the ideal candidate for LIMA to LAD graft?
Patients with blockages in the left anterior descending artery, especially those with diabetes or reduced heart function, benefit most from this graft due to its durability and excellent outcomes.
Are there risks associated with bypass surgery?
As with any major surgery, risks include bleeding, infection, stroke, or heart attack during or after the procedure. However, advances in technology and care have significantly reduced these risks.
Can bypass surgery cure coronary artery disease?
Bypass surgery improves blood flow and symptoms but does not cure the underlying disease. Lifestyle changes and medications are essential to manage the condition long-term.
What is off-pump bypass surgery?
Off-pump bypass surgery is performed without stopping the heart or using a heart-lung machine, potentially reducing complications in selected patients.
Is robotic bypass surgery widely available?
Robotic-assisted bypass surgery is available in specialized centers and offers minimally invasive options but is not yet widespread due to technical and cost considerations.