Heart disease remains one of the leading causes of mortality worldwide, and many patients face critical decisions regarding their treatment options. Among these, two of the most common interventions to restore blood flow to the heart are stent placement and bypass surgery. But a question that often arises is: Are these procedures permanent cures? Do they guarantee a lifetime free from heart problems, or is there a risk of recurrence? In this comprehensive article, we delve deeply into these questions, drawing from the expertise of Dr. Nagendra Boopathy, a leading cardiologist who explains the nuances of stents and bypass surgery in Tamil, making complex cardiac care concepts accessible.
Understanding Stents: What Are They and How Do They Work?
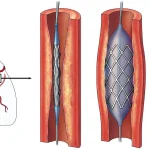
A stent is essentially a small metallic tube inserted into a narrowed or blocked coronary artery to keep it open and ensure proper blood flow to the heart muscle. There are two main types of stents used in cardiac care:
- Metallic Stents: These are traditional bare metal stents that provide structural support to the artery but lack any drug coating.
- Drug-Eluting Stents (DES): These stents are coated with medication that slowly releases into the artery to prevent scar tissue formation and reduce the chances of re-narrowing (restenosis).
Dr. Boopathy highlights that drug-eluting stents have proven to be more effective than bare metal stents, especially in preventing restenosis. However, even with the best stents, outcomes vary from patient to patient.
How Long Does a Stent Last?
One of the most frequently asked questions is about the longevity of stents. While the goal is for a stent to last a lifetime, reality is more complex. According to Dr. Boopathy, approximately 90 to 95% of stents function well over time. However, 5 to 10% of patients may experience complications, especially those with underlying conditions like diabetes or a history of heart attacks.
These complications often manifest as restenosis or blockage at the stent site, which can occur months or even years after the initial procedure. Factors contributing to this include:
- Calcium build-up around the stent
- Blood clot formation
- Progression of atherosclerosis in other parts of the coronary arteries
Patients who have multiple stents, especially in complex cases like bifurcation lesions (where two arteries branch), may have a higher risk of restenosis.
Importance of Proper Stent Deployment and Follow-Up
Dr. Boopathy stresses that the success of a stent procedure depends heavily on how well the stent is deployed. Poorly expanded or improperly positioned stents increase the risk of restenosis. To ensure optimal results, advanced imaging techniques such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT) are used. These tools allow cardiologists to visualize the artery from inside and confirm that the stent is fully expanded and apposed to the vessel wall.
Regular follow-up and monitoring are essential to detect any signs of re-narrowing early and to intervene promptly if necessary.
Bypass Surgery: What Does It Involve?
Bypass surgery, also known as coronary artery bypass grafting (CABG), involves taking a healthy blood vessel from another part of the body and grafting it to bypass the blocked coronary artery, restoring blood flow to the heart muscle.
There are two main types of bypass grafts commonly used:
- Left Internal Mammary Artery (LIMA) to Left Anterior Descending (LAD) Artery Graft: This graft uses an artery from the chest wall, which has excellent long-term patency rates.
- Vein Grafts (e.g., Saphenous Vein Graft or SVG): These are taken from the leg and used to bypass other blocked arteries.
Graft Longevity and Success Rates
Dr. Boopathy explains that while LIMA to LAD grafts have a high success rate and can remain open for many years, vein grafts tend to have a higher rate of failure over time. Statistics show:
- Approximately 10% of vein grafts may become blocked soon after surgery.
- About 25% may fail within the first year.
- Over the years, the failure rate increases, with up to 50% of vein grafts potentially becoming occluded within 10 years.
This variability means that bypass surgery, while highly effective, is not always a permanent fix. The risk of graft failure and progression of disease in native coronary arteries necessitates continued medical management and lifestyle modifications.
Advancements: Arterial Grafts and Their Advantages
To overcome the limitations of vein grafts, surgeons have increasingly used arterial grafts, such as the radial artery or other arterial conduits, which have better durability and lower failure rates. Long-term studies indicate that arterial grafts maintain better patency, with around 80% remaining open even after 8 to 10 years.
However, even with arterial grafts, the risk of developing new blockages elsewhere in the heart or graft failure exists, underscoring the importance of ongoing care.
Stent vs. Bypass: Which Is the Better Option?
Choosing between stenting and bypass surgery depends on multiple factors including the extent and location of artery blockages, patient’s overall health, presence of diabetes, heart function, and patient preference.
- Single or less complex blockages: Stenting is often preferred due to its minimally invasive nature and quicker recovery.
- Multiple or complex blockages: Bypass surgery is generally recommended, especially if the left main coronary artery or multiple vessels are involved.
- Diabetic patients: May benefit more from bypass surgery because of better long-term outcomes compared to stenting.
Dr. Boopathy emphasizes that there is no one-size-fits-all answer. Each patient’s unique condition and risk profile must be carefully evaluated by the cardiology team to determine the best course of action.
What Happens When Blockages Recur?
Both stents and bypass grafts can develop blockages over time. When this occurs, the treatment approach depends on the severity, location, and symptoms:
- Repeat angioplasty and stenting: This may be possible if the blockage is suitable for another minimally invasive procedure.
- Second bypass surgery: Sometimes considered, but it carries higher risks and is less commonly performed.
- Medical management: In some cases, symptoms can be controlled with medications and lifestyle changes without immediate intervention.
Decisions are individualized, balancing the risks and benefits of further interventions.
The Role of Lifestyle and Medical Therapy After Procedures
One of the most critical points Dr. Boopathy makes is that neither stenting nor bypass surgery is a standalone cure. These procedures address the immediate problem of blocked arteries but do not halt the underlying disease process — atherosclerosis.
To maximize the longevity and effectiveness of these treatments, patients must:
- Adhere to prescribed medications: Including antiplatelet drugs, cholesterol-lowering agents (statins), blood pressure medications, and diabetes control medications if applicable.
- Maintain a heart-healthy lifestyle: This includes a balanced diet low in saturated fats and sugars, regular physical activity, quitting smoking, and managing stress.
- Regular follow-ups: Monitoring with the cardiologist to detect any changes early and adjust treatment accordingly.
Ignoring these measures increases the risk of restenosis, graft failure, and new blockages, which can lead to heart attacks or other serious complications.
Advanced Imaging Techniques to Monitor Stent and Graft Health
To ensure stents are functioning well and grafts remain patent, cardiologists use advanced intravascular imaging tools:
- Intravascular Ultrasound (IVUS): Provides cross-sectional images from inside the artery to assess stent expansion and vessel wall characteristics.
- Optical Coherence Tomography (OCT): Offers high-resolution images to detect even subtle changes around the stent.
Using these technologies during and after procedures helps minimize the risk of restenosis and guides timely interventions if needed, improving long-term outcomes.
Summary: What Have We Learned About Stents and Bypass Surgery?
Both stent placement and bypass surgery are powerful tools in the fight against coronary artery disease. However, neither is a guaranteed permanent cure. The success and longevity of these interventions depend on multiple factors including the type of stent or graft used, patient’s overall health, and strict adherence to medical and lifestyle recommendations.
Key takeaways include:
- Drug-eluting stents have improved outcomes but still carry a risk of restenosis, especially in diabetic patients.
- Bypass surgery, particularly with arterial grafts like the LIMA to LAD, offers durable results but vein grafts may fail over time.
- Recurrence of blockages is possible with both treatments, necessitating ongoing monitoring and sometimes repeat interventions.
- Optimal results require lifelong commitment to medications, healthy living, and regular medical follow-up.
Ultimately, decisions regarding stenting or bypass surgery should be personalized, made in consultation with experienced cardiologists who consider all clinical factors and patient preferences.
Frequently Asked Questions (FAQs)
1. Is a stent a permanent solution to heart artery blockage?
No. While stents, especially drug-eluting ones, significantly reduce the risk of artery re-narrowing, they are not a guaranteed permanent cure. There is still a 5 to 10% chance of restenosis depending on individual risk factors.
2. How long does a bypass graft last?
Arterial grafts like the LIMA to LAD can last 10 years or more with good patency rates. Vein grafts have a higher failure rate, with up to 50% possibly becoming blocked within 10 years.
3. Can blockages return after bypass surgery or stenting?
Yes, blockages can recur due to progression of atherosclerosis or graft failure. This is why ongoing medical management and lifestyle changes are vital.
4. What are the risks of repeat procedures after stent or bypass failure?
Repeat angioplasty and stenting are often possible and less risky than repeat bypass surgery, which carries higher surgical risks and is less commonly performed.
5. What lifestyle changes help improve the success of stents and bypass surgery?
Maintaining a healthy diet, regular exercise, quitting smoking, controlling blood sugar and blood pressure, and adhering to prescribed medications are essential to prolong the benefits of these procedures.
6. How do doctors check if a stent or bypass graft is working well?
Advanced imaging techniques like intravascular ultrasound (IVUS) and optical coherence tomography (OCT) help visualize stents and grafts to ensure they are functioning properly.
Final Thoughts
Heart disease management is a journey rather than a one-time fix. Stents and bypass surgeries are critical interventions that save lives and improve quality of life, but they are part of a broader treatment plan. Patients must partner closely with their healthcare providers, follow medical advice diligently, and embrace lifestyle changes to ensure these treatments offer the maximum possible benefit over time.
By understanding the strengths and limitations of stents and bypass surgery, patients can make informed decisions and set realistic expectations for their heart health. As Dr. Nagendra Boopathy advises, regular medication adherence, lifestyle control, and medical follow-up are the cornerstones of successful long-term cardiac care.
Take charge of your heart health today and work with your cardiologist to choose the best treatment plan tailored for you.
Dr. S Nagendra Boopathy
Schedule an Appointment:
- Link: Schedule Here
- Instructions: Select the date and time below to schedule an appointment.
For Appointment Confirmation and Follow-Ups, Please Contact:
- 9 AM – 4 PM: +919360438720
- 6 PM – 8 PM: +918754498680
Ensure all details are verified after scheduling your appointment.