Angioplasty is a well-known procedure in the field of cardiology, widely used to treat blockages in coronary arteries and restore blood flow to the heart. However, the medical community has continuously evolved this technique to enhance precision, safety, and patient outcomes. One such advancement is Image Guided Angioplasty, a cutting-edge approach that combines traditional angioplasty with sophisticated imaging technologies to optimize treatment, especially in complex cases.
In this article, we will explore the concept of Image Guided Angioplasty, its differences from conventional angioplasty, the imaging modalities involved, and why it represents a significant leap forward in cardiac intervention. The insights presented here are based on expert explanations by Dr. S. Nagendra Boopathy, a renowned Interventional Cardiologist at Sri Ramachandra Medical College and Heart Care, Chennai.
What is Angioplasty?
Before diving into the advanced technique of Image Guided Angioplasty, it’s important to understand the basics of traditional angioplasty. Angioplasty, also called Percutaneous Coronary Intervention (PCI), is a minimally invasive procedure designed to open narrowed or blocked coronary arteries to improve blood flow to the heart muscle.
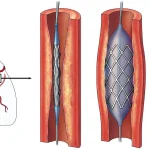
Typically, a thin wire is threaded through a blood vessel, either via the wrist or the groin, to reach the blocked artery in the heart. A balloon catheter is then inflated at the site of the blockage to dilate the artery, and a stent—a tiny mesh tube—is often placed to keep the artery open permanently.
This procedure has been a cornerstone of cardiac care for decades, saving countless lives and reducing symptoms such as chest pain (angina) and the risk of heart attacks. However, traditional angioplasty relies heavily on X-ray fluoroscopy to visualize the blood vessels and guide the intervention.
Introducing Image Guided Angioplasty
Image Guided Angioplasty takes the procedure a step further by incorporating advanced imaging techniques during the intervention. Unlike standard angioplasty, which primarily uses X-ray images, this approach integrates real-time, high-resolution imaging methods such as Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT). These technologies enable cardiologists to see detailed cross-sectional images of the blood vessels from inside, providing critical information about the plaque characteristics, vessel size, and stent placement.
Dr. Boopathy explains that Image Guided Angioplasty is essentially an upgrade to the traditional method. It is particularly useful in complex coronary artery disease cases where precision is crucial. By using ultrasound waves or near-infrared light waves inside the artery, doctors can assess:
- The exact location and extent of blockages
- The composition of the plaque, including calcium deposits
- The severity and length of the lesion
- How well the balloon and stent expand within the artery
This detailed visualization helps optimize the procedure, ensuring that the stent is placed accurately and fully expanded, which reduces the chances of complications like restenosis (re-narrowing of the artery) or stent thrombosis (clot formation).
Imaging Modalities Used in Image Guided Angioplasty
Intravascular Ultrasound (IVUS)
IVUS involves inserting a tiny ultrasound probe mounted on a catheter into the coronary artery. This probe emits sound waves that bounce off the artery walls and plaques, creating real-time images. IVUS can reveal the thickness of the arterial wall, the amount of calcium, and the degree of narrowing, which are not always apparent on conventional X-ray images.
Optical Coherence Tomography (OCT)
OCT uses near-infrared light to generate high-resolution images of the artery’s interior. It offers even more detailed visualization than IVUS, allowing doctors to see microstructures within the plaque and stent. OCT is especially valuable for assessing stent apposition (how well the stent fits against the artery wall) and detecting subtle complications.
Both IVUS and OCT complement the traditional X-ray angiography, providing a comprehensive picture that guides the intervention with precision.
Why Image Guided Angioplasty is a Game Changer
The recent scientific community has recognized the immense value of Image Guided Angioplasty in improving patient outcomes. According to Dr. Boopathy, studies and clinical guidelines, including those set to be updated in 2025, emphasize that this technique should be considered a must-do in complex angioplasty cases.
Here are some of the key benefits of Image Guided Angioplasty:
- Improved Accuracy: Real-time imaging allows cardiologists to precisely identify the problem areas and tailor the treatment accordingly.
- Optimized Stent Placement: Ensures the stent is fully expanded and apposed to the artery walls, minimizing the risk of future complications.
- Better Long-Term Outcomes: Patients experience fewer adverse events such as restenosis, leading to improved heart function and quality of life.
- Enhanced Safety: Detailed imaging reduces the chances of procedural errors and complications.
- Useful in Complex Cases: Particularly beneficial in arteries with bifurcations (where a vessel splits into two) or heavy calcification.
Dr. Boopathy also highlights that while the global adoption of Image Guided Angioplasty has been gradual, it is steadily increasing due to its proven benefits. Initially, less than 20% of angioplasty procedures worldwide used intravascular imaging, but this number is growing as more cardiologists recognize its importance.
How Does Image Guided Angioplasty Work in Practice?
During the procedure, after the initial angiogram (X-ray imaging of the arteries), the cardiologist introduces the intravascular imaging catheter into the artery. This catheter provides detailed images of the lesion and vessel, helping to decide the appropriate balloon size, stent length, and deployment technique.
The cardiologist can then perform the balloon dilation and stent placement while continuously monitoring the artery’s response through the imaging device. This dynamic feedback loop allows for immediate adjustments, such as additional balloon inflations or stent repositioning, to achieve optimal results.
After the stent is deployed, the imaging catheter is used again to confirm that the stent is well expanded and there are no residual narrowings or complications. This thorough evaluation is critical for ensuring the success of the procedure and the long-term health of the patient.
Image Guided Angioplasty vs. Traditional Angioplasty
| Aspect | Traditional Angioplasty | Image Guided Angioplasty |
|---|---|---|
| Imaging | X-ray fluoroscopy only | X-ray plus intravascular ultrasound or optical coherence tomography |
| Visualization | 2D images, limited plaque characterization | 3D cross-sectional images with detailed plaque and vessel wall info |
| Stent Placement | Based on angiogram images, less precise | Guided by detailed imaging for optimal expansion and positioning |
| Outcome | Good, but risk of restenosis or stent issues higher | Improved long-term patency and reduced complications |
| Usefulness | Effective for simple cases | Especially valuable in complex anatomy and lesions |
Future Perspectives and Clinical Guidelines
With ongoing research and technological advancements, Image Guided Angioplasty is becoming the new standard of care in interventional cardiology. Leading cardiology societies worldwide are updating their guidelines to recommend intravascular imaging as part of routine practice, especially in complex cases.
Dr. Boopathy mentions that the 2025 guidelines will emphasize this technique as a must-do procedure, reflecting the strong scientific evidence supporting its benefits. This shift will likely lead to broader adoption and training in Image Guided Angioplasty, improving patient care globally.
Conclusion
Image Guided Angioplasty represents a significant advancement in the treatment of coronary artery disease. By combining traditional angioplasty with sophisticated intravascular imaging techniques such as IVUS and OCT, cardiologists can perform more precise, safer, and effective interventions.
This approach not only improves the immediate success of the procedure but also enhances long-term outcomes for patients, reducing the risk of complications and improving heart health. As clinical guidelines evolve to incorporate these technologies, Image Guided Angioplasty is poised to become the gold standard in complex cardiac interventions.
If you or a loved one is facing angioplasty, discussing the possibility of Image Guided Angioplasty with your cardiologist could provide additional reassurance and better results.
Frequently Asked Questions (FAQ)
What is the main difference between traditional angioplasty and Image Guided Angioplasty?
Traditional angioplasty relies mainly on X-ray imaging to guide the procedure, while Image Guided Angioplasty uses advanced intravascular imaging techniques like ultrasound and optical coherence tomography to provide detailed, real-time views of the artery from inside. This allows for more precise treatment.
Is Image Guided Angioplasty safe?
Yes, it is safe and is associated with better procedural accuracy and fewer complications. The additional imaging helps cardiologists avoid errors and optimize stent placement.
Who benefits most from Image Guided Angioplasty?
Patients with complex coronary artery disease, such as those with bifurcation lesions or heavy calcification, benefit the most. However, it is increasingly being used in a wider range of cases due to its advantages.
Does Image Guided Angioplasty take longer than traditional angioplasty?
The procedure may take slightly longer because of the additional imaging steps, but this is outweighed by improved outcomes and reduced need for repeat interventions.
Is Image Guided Angioplasty widely available?
While it is becoming more common, especially in advanced cardiac centers, the adoption varies globally. Awareness and training are increasing, leading to broader availability.
Are there any additional costs involved with Image Guided Angioplasty?
There may be some additional costs for the imaging equipment and catheters, but these are often justified by the improved safety and long-term benefits.
About Dr. S. Nagendra Boopathy
Dr. S. Nagendra Boopathy is a Professor of Cardiology and a Consultant Cardiologist at Sri Ramachandra Medical College and Heart Care, Kodambakkam, Chennai. With qualifications including MBBS from Madras Medical College, MD in Internal Medicine, and DM in Cardiology from prestigious institutes, Dr. Boopathy specializes in interventional cardiology. His expertise and dedication to advancing cardiac care have made him a trusted name in the field.
For more expert insights on heart health and the latest advancements in cardiology, you can follow Dr. Boopathy’s Heart Care channel and resources.