Aortic stenosis is a serious heart condition that requires attention and understanding. This article delves into the intricacies of aortic stenosis, providing insights into its causes, symptoms, diagnosis, and treatment options. By gaining a thorough understanding of this condition, individuals can better manage their health and make informed decisions.
What is Aortic Stenosis?
Aortic stenosis occurs when the aortic valve narrows, hindering blood flow from the heart to the rest of the body. This condition can lead to significant health issues, including heart failure if left untreated. Understanding the anatomy and function of the aortic valve is crucial for grasping the implications of aortic stenosis.
The Anatomy of the Aortic Valve
The aortic valve is one of four valves in the heart, located between the left ventricle and the aorta. It plays a vital role in ensuring that blood flows in one direction, preventing backflow into the heart. The valve opens to allow blood to leave the heart and closes to maintain pressure within the heart. When this valve becomes narrowed, the heart must work harder to pump blood, leading to various complications.
Causes of Aortic Stenosis
Aortic stenosis can arise from several factors, typically categorized into congenital and acquired causes. Understanding these causes is essential for prevention and early detection.
Congenital Causes
- Congenital Heart Defects: Some individuals are born with aortic valves that have only two leaflets instead of the normal three, a condition known as congenital bicuspid aortic valve.
Acquired Causes
- Age-Related Calcification: As individuals age, calcium deposits can accumulate on the aortic valve, causing it to stiffen and narrow.
- Rheumatic Fever: A history of rheumatic fever can lead to scarring of the aortic valve, contributing to stenosis.
- Radiation Therapy: Previous radiation treatment to the chest can also affect the aortic valve and lead to stenosis.
Symptoms of Aortic Stenosis
Recognizing the symptoms of aortic stenosis is crucial for timely intervention. Symptoms may develop gradually and can sometimes be mistaken for other conditions.
Common Symptoms
- Shortness of Breath: Patients often experience breathlessness during physical activity or even at rest.
- Chest Pain: Discomfort or pain in the chest may occur, particularly during exertion.
- Fatigue: A general feeling of tiredness or weakness can be a red flag.
- Dizziness or Fainting: Some individuals may feel lightheaded or faint, especially during physical activities.
Advanced Symptoms
If aortic stenosis progresses, symptoms can worsen, leading to more severe complications. These may include:
- Severe chest pain
- Heart palpitations
- Heart failure symptoms, such as swelling in the legs and ankles
Diagnosing Aortic Stenosis
Diagnosing aortic stenosis involves a combination of medical history, physical examination, and diagnostic tests. Early detection is key to effective management.
Medical History and Physical Examination
A healthcare provider will begin by taking a detailed medical history and performing a physical examination. They will listen for characteristic heart murmurs, which can indicate the presence of aortic stenosis.
Diagnostic Tests
- Echocardiogram: This ultrasound test provides images of the heart and can assess the severity of the stenosis.
- Electrocardiogram (ECG): An ECG measures the electrical activity of the heart and can reveal any irregularities.
- Chest X-ray: This imaging test can help visualize the heart’s size and the condition of the aortic valve.
- Cardiac Catheterization: In some cases, this invasive procedure may be necessary to gather more detailed information about the heart’s function.
Treatment Options for Aortic Stenosis
Treatment for aortic stenosis depends on the severity of the condition and the presence of symptoms. Options range from monitoring to surgical interventions.
Monitoring
In cases where aortic stenosis is mild and asymptomatic, regular monitoring may be sufficient. Healthcare providers will schedule periodic check-ups to assess the condition.
Medications
While no medications can reverse aortic stenosis, certain drugs may help manage symptoms or associated conditions. These can include:
- Diuretics: To help reduce fluid retention.
- Beta-blockers: To manage heart rate and blood pressure.
Surgical Interventions
When symptoms are present or the condition is severe, surgical intervention is often necessary. Two primary surgical options are:
Aortic Valve Replacement
This is the most common treatment for severe aortic stenosis. The damaged valve is replaced with a mechanical or biological valve. This procedure can be done through traditional open-heart surgery or minimally invasive techniques.
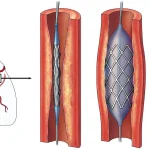
Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a newer, less invasive procedure suitable for patients who are at high risk for traditional surgery. A catheter is used to insert a replacement valve through the blood vessels, typically via the femoral artery.
Living with Aortic Stenosis
Managing life with aortic stenosis involves regular check-ups and lifestyle modifications. Following a healthcare provider’s recommendations is essential for maintaining heart health.
Lifestyle Modifications
- Diet: A heart-healthy diet can help manage symptoms and improve overall cardiovascular health.
- Exercise: Regular physical activity, as advised by a healthcare provider, can strengthen the heart.
- Avoiding Smoking: Quitting smoking is crucial for heart health.
Regular Monitoring
Regular follow-ups with a cardiologist are essential for monitoring the condition. This ensures prompt management of any changes in symptoms or condition severity.
FAQs on Aortic Stenosis
1. What is aortic stenosis?
Aortic stenosis is a condition where the aortic valve, located between the left ventricle and the aorta, becomes narrowed. This narrowing restricts blood flow from the heart to the rest of the body, forcing the heart to work harder to pump blood.
2. What causes aortic stenosis?
Aortic stenosis can be caused by congenital heart defects, age-related calcification of the aortic valve, or a history of rheumatic fever. The most common cause in older adults is the accumulation of calcium deposits on the valve over time.
3. What are the symptoms of aortic stenosis?
Symptoms of aortic stenosis can include chest pain (angina), shortness of breath, fatigue, palpitations, dizziness, or fainting (syncope). These symptoms may worsen over time as the condition progresses.
4. How is aortic stenosis diagnosed?
Aortic stenosis is typically diagnosed through an echocardiogram, which provides detailed images of the heart and aortic valve. Additional tests, such as an electrocardiogram (ECG), cardiac catheterization, or CT/MRI scans, may also be used to assess the severity of the condition.
5. Can aortic stenosis be treated with medication?
While medications can help manage symptoms of aortic stenosis, they do not cure the condition or stop its progression. Treatment usually involves procedures to repair or replace the narrowed valve.
6. What is Transcatheter Aortic Valve Replacement (TAVR)?
TAVR is a minimally invasive procedure used to replace a narrowed aortic valve. It involves inserting a catheter through the femoral artery and deploying a new valve within the existing one. TAVR is often recommended for patients who are at high risk for traditional open-heart surgery.
7. What is the difference between TAVR and Surgical Aortic Valve Replacement (SAVR)?
TAVR is a less invasive procedure performed through a catheter, making it suitable for high-risk patients. SAVR is a traditional open-heart surgery where the damaged valve is replaced with a mechanical or biological valve. SAVR is often recommended for patients who are fit for surgery.
8. Is aortic stenosis hereditary?
Aortic stenosis can have a genetic component, particularly in cases involving congenital heart defects like a bicuspid aortic valve. However, age-related calcification is the most common cause and is not typically hereditary.
9. What happens if aortic stenosis is left untreated?
If left untreated, aortic stenosis can lead to severe complications, including heart failure, arrhythmias, and sudden cardiac death. It is crucial to seek medical attention and consider treatment options if diagnosed with this condition.
10. How long is the recovery time after TAVR or SAVR?
Recovery time varies depending on the procedure and the patient’s overall health. Patients undergoing TAVR typically experience a shorter recovery period, often returning to normal activities within a few weeks. Recovery from SAVR may take several weeks to months, depending on the individual case.
11. Can lifestyle changes help manage aortic stenosis?
While lifestyle changes such as maintaining a healthy diet, exercising regularly, and managing blood pressure can support overall heart health, they cannot reverse or cure aortic stenosis. These changes may help manage symptoms and improve quality of life.
12. When should I see a specialist for aortic stenosis?
You should see a cardiologist if you experience symptoms such as chest pain, shortness of breath, or fainting, especially if you have risk factors for heart disease. Early diagnosis and treatment can significantly improve outcomes.
13. What makes Dr. S. Nagendra Boopathy a leading expert in aortic stenosis treatment?
Dr. S. Nagendra Boopathy is a renowned interventional cardiologist with extensive experience in treating aortic stenosis. His expertise in advanced procedures like TAVR, SAVR, and other interventional cardiology techniques ensures that patients receive the most effective and personalized care.
14. How can I schedule a consultation with Dr. S. Nagendra Boopathy?
To schedule a consultation with Dr. S. Nagendra Boopathy, you can contact his clinic directly through the provided phone number or visit his website to book an appointment online. Early consultation is key to receiving timely and appropriate care for aortic stenosis.